By Dr. Aswin Babu
Edited by Dr. Ahmed El-Medany
The evidence and landscape around anti-platelet and anticoagulation strategies for established coronary disease continues to evolve and advance at a rapid rate. Thus, the need for a complete document analysing the current contemporary evidence is essential in providing physicians a template for optimal care.
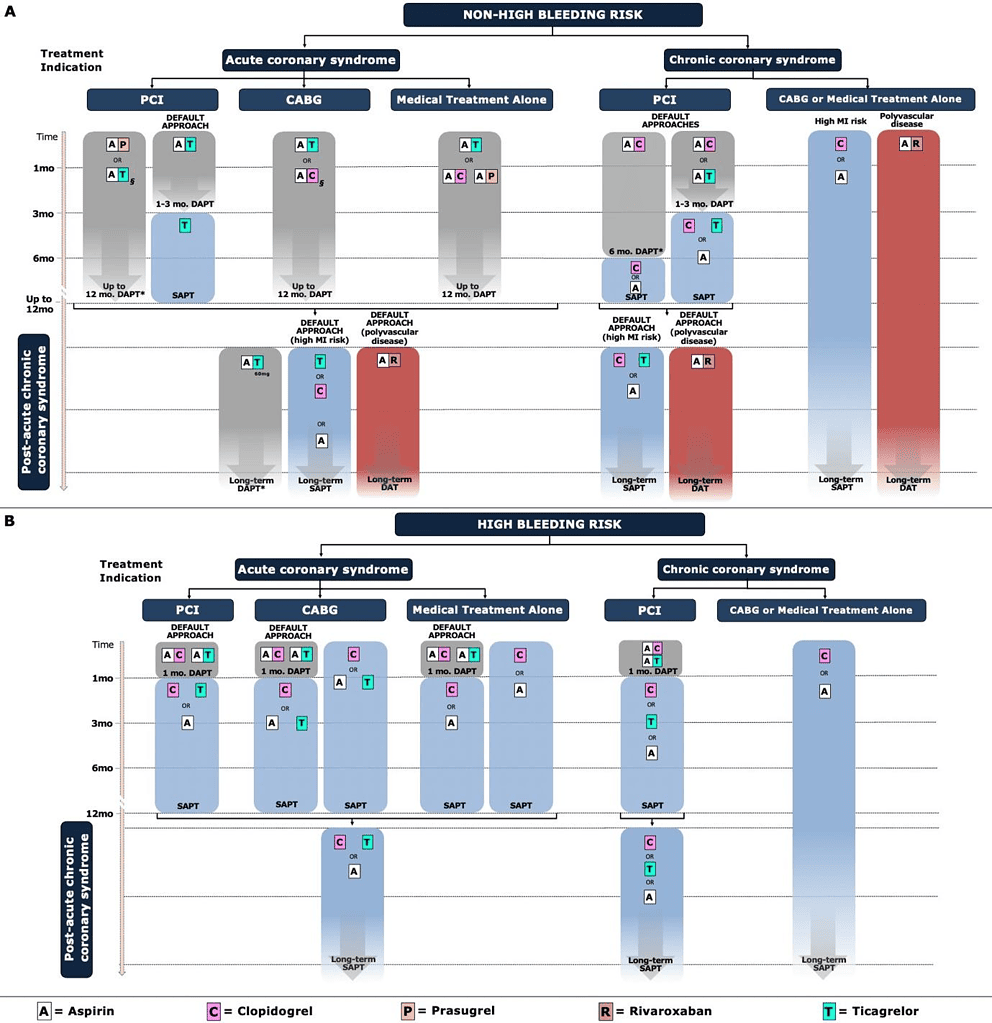
Figure 1 – Schema outlining antithrombotic regimens for the whole spectrum of coronary artery disease. Taken from Valgimigli et al (2023) https://shorturl.at/hiDY4.
Key points covered by the document include:
- Patients at high bleeding risk (HBR) is defined based on the Academic Research Consortium (ARC)-HBR criteria or a PRECISE-DAPT score ≥ 25.
- The MASTERDAPT trial demonstrated a net clinical benefit for 1-month duration of DAPT in both ACS (48%) and non-ACS patients at HBR undergoing PCI by meeting non-inferiority for MACE and cerebral event end points when compared to standard DAPT duration (> 3 months). Yet in the STOPDAPT2-ACS trial, clopidogrel monotherapy after 1 month of DAPT did not meet non-inferiority for the composite end point of cardiovascular death, MI, definite stent thrombosis, and stroke. This was mainly due to the significantly higher rates of MI in the clopidogrel monotherapy arm.
- ACS patients undergoing revascularisation with CABG should have DAPT for up to 12 months unless concerns over HBR prevail. Aspirin plus ticagrelor provides a greater ischaemic protection when compared to aspirin plus clopidogrel.
- In patients with ACS who are medically managed, aspirin in addition to ticagrelor has been shown to achieve superior outcomes in ischemic endpoints without a significant increase in bleeding risk when compared to aspirin plus clopidogrel. However, observational data suggests that caution must be undertaken in octogenarians.
- Patients at HBR should not exceed 1 month duration of DAPT irrespective of complex anatomy or number of stents.
- Network meta-analysis examining 43 (n = 189,261 patients) trials within 12 months and 19 (n = 139,086 patients) trials beyond 12 months after PCI or ACS (including medically managed), revelaed that ticagrelor monotherapy demonstrated lower mortality without a substantial bleeding risk when compared to aspirin and clopidogrel in each time frame.
- Aspirin in combination with low dose rivaroxaban (2.5mg bd) after initial DAPT has been shown to be the most effective treatment strategy in reducing stroke when compared to other antithrombotic strategies. This should be the default treatment mode in patients with polyvascular disease and prior stroke. However, there is a higher risk of major and intracranial bleeding with this regimen.
- Furthermore, low dose rivaroxaban plus aspirin can be used in patients with chronic coronary syndromes at high ischemic but low bleeding risk independent of the revascularisation strategy.
- 12 months post myocardial infarction, P2Y12 monotherapy in the form of either clopidogrel (CAPRIE, HOST-EXAM) or ticagrelor (TICO, TWILIGHT, Network meta-analysis) has been shown to have enhanced ischaemic outcomes without increased bleeding risk when compared to aspirin alone.
- In individuals with a prior MI with a high ischaemic but low bleeding risk, the PEGASUS-TIMI 54 trial showed benefit for the use of ticagrelor 60mg bd + aspirin for up to 2 years post initial DAPT regimen compared to aspirin alone with a significant reduction in cardiovascular death, MI, or stroke.
- A prolonged duration of DAPT (> 12 months) has not shown any net benefit in patients undergoing PCI for angina. P2Y12 monotherapy (Clopidogrel or Ticagrelor) when rivalled to aspirin after initial DAPT provides the most significant net clinical benefit.
- In bypass patients without previous MI, clopidogrel monotherapy provides a net clinical benefit when compared with aspirin but there is currently no role for DAPT.
- In patients with chronic coronary syndromes who are managed medically, clopidogrel or aspirin monotherapy use can be justified in symptomatic patients. Once again, there is currently no role for DAPT.
- To date, there is no convincing evidence or RCT supporting the role of platelet function testing for guiding P2Y12 inhibitor treatment in improving outcomes in patients undergoing PCI for either ACS or CCS.
Link to article
https://academic.oup.com/ehjcvp/advance-article/doi/10.1093/ehjcvp/pvad032/7147298