By Dr. Timothy Swinn
A study recently published in Plos Medicine by Rezel-Potts et al1 has shown that the incidence of diabetes and cardiovascular conditions remains increased, compared to baseline, for at least 12 weeks after acute covid-19 infection. Their secondary analysis suggests that this increased incidence may even persist for up to 20-23 weeks post infection for diabetes.
The authors conducted a cohort study using an electronic record from UK GP practices. They included 428,650 patients with clinical or proven diagnosis of acute covid-19 infection and matched this with controls. Subjects were excluded if they had a diagnosis of diabetes more than 1 year prior to infection. Data were analysed for 1 year prior to covid infection/index date so that baseline rates of diabetes and cardiovascular incidence could be established for both groups. Primary analysis grouped the post infection timeline into 3 categories: 4 weeks from index date (“acute COVID-19”), 5-12 weeks from index date (“post-acute COVID-19”), and 13-52 weeks from index date (“long COVID-19”).
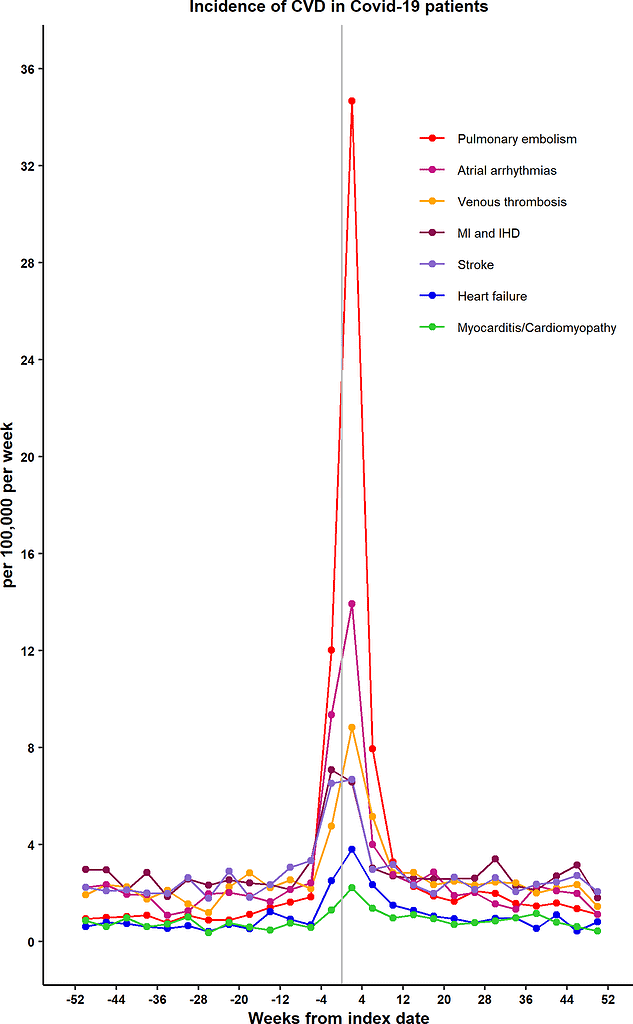
The authors found that diabetes diagnosis incidence was increased in acute COVID-19 (adjusted relative rate (RR) 1.81, 95% confidence interval (CI) 1.51-2.19) and post-acute COVID-19 (RR 1.27 (1.11-1.46)) but returned to baseline in long COVID-19. Cardiovascular disease incidence was also increased in these time frames (figure 1- taken from Rezel-Potts et al 20221. This was primarily driven in acute COVID-19 by an increase in pulmonary embolism (RR 11.51 (7.07-18.83)), atrial arrhythmia (RR 6.44 (4.17-9.96)), venous thrombosis (RR 5.43 (3.27-9.01)), and heart failure (RR 5.23 (2.04-13.44)). The incidence of these diagnoses remained increased in post-acute COVID-19 but to a lesser degree (PE: RR 2.29 (1.47-3.57), atrial arrhythmia: RR 1.58 (1.10-2.27), venous thrombosis: RR 1.84 (1.27-2.64), heart failure: RR 2.30 (1.17-4.51)), but returned to baseline rates for long COVID-19. Secondary analysis by timeframe in 4-week increments suggested that the diabetes diagnosis incidence only returned to baseline levels in the 24-27 weeks post infection timeframe.
Authors analysed the prescription of glucocorticoids and corrected for increased consultation frequency in the COVID-19 group. Neither of these factors is expected to explain the difference in diabetes incidence.
Whilst this cohort study cannot infer causality, the authors acknowledged possible mechanisms for the increase in diabetes incidence; this could be due to SARS-CoV-2 causing impaired insulin secretion or insulin resistance, or simply unmasking an existing but undiagnosed condition. The study shows that incidence of significant diagnoses persists several weeks after acute infection. This requires further investigation into possible mechanisms and may lead to heightened surveillance of susceptible patients.
Figure 1
Increase in incidence of cardiovascular conditions after acute COVID-19 infection.
References:
- Rezel-Potts E, Douiri A, Sun X, Chowienczyk PJ, Shah AM, Gulliford MC. Cardiometabolic outcomes up to 12 months after COVID-19 infection. A matched cohort study in the UK. PLOS Med. 2022 Jul 19;19(7):e1004052.